Bladder prolapse: a common cause of incontinence
What is bladder prolapse?
Bladder prolapse (prolapsed bladder, cystocele) occurs when the bladder is displaced downwards towards the pelvic floor and backwards.
For anatomical reasons, bladder prolapse only affects women, as it is caused by an overstretching or slackening of the bladder support system consisting of muscles, ligaments and connective tissue. Urinary incontinence and frequent bladder infections are typical complications of a prolapsed bladder.However, a pronounced prolapse of the bladder can also be treated well using various methods.
The doctors at the Hirslanden Continence Centre in Zurich specialize in the examination and treatment of bladder prolapse.
Please make an appointment at our center and we will inform you about your individual examination and treatment options.
Find out now about the diagnosis and treatment of bladder prolapse
A bladder prolapse is usually very treatable. Contact us for a consultation — we will be happy to inform you about your individual treatment options.
Causes: How does bladder prolapse occur?
 Bladder prolapse is often caused by loosening and stretching of the holding apparatus: In the female pelvis, a number of organs are located in close proximity to each other and to the bladder: The bladder and urethra are located directly behind the pubic bone at the front, the uterus and vagina in the middle and the rectum at the back towards the sacrum.
Bladder prolapse is often caused by loosening and stretching of the holding apparatus: In the female pelvis, a number of organs are located in close proximity to each other and to the bladder: The bladder and urethra are located directly behind the pubic bone at the front, the uterus and vagina in the middle and the rectum at the back towards the sacrum.
All of these organs, including the bladder, are connected to the pelvic bones and also to each other by muscles, ligaments and connective tissue structures.
The main cause of bladder prolapse is weakened pelvic floor muscles.
This is mainly favored by:
- Pregnancies and births
- Loads such as heavy lifting
- Menopause and age
- Overweight
- Chronic constipation
- Chronic cough disease
Pregnancy and childbirth promote bladder prolapse
An aggravating factor for bladder prolapse is the heavy strain placed on the connective tissue ligaments in the course of life, especially during pregnancy and childbirth. During pregnancy, the uterus increases significantly in size and weight, putting a lot of strain and stretching on the ligaments. There is even a risk of one or more ligaments tearing. The muscles and ligaments holding the bladder, vagina and uterus can also be loosened or even torn during childbirth, leading to bladder prolapse.
In addition, the female pelvic floor muscles need to be much more flexible for childbirth than the male pelvic floor muscles. After a birth, the entire holding apparatus, including the supporting muscles, often no longer fully regenerates. The risk of bladder prolapse therefore increases with the number of births, or an existing prolapse can be exacerbated. In addition to bladder prolapse, the weakened pelvic floor muscles often lead to other organ prolapse in the pelvis, such as vaginal or uterine prolapse.
Additional risk factors
In women with connective tissue weakness, everyday strain over the years can lead to loosening and stretching of the supporting structures — and consequently to a bladder prolapse — even without having given birth. After menopause, a prolapse of the bladder, uterus, and/or rectum may develop, potentially influenced by hormonal factors and weight gain.
Symptoms: What are the effects of bladder prolapse?
Mild bladder prolapse can often be symptom-free and therefore often goes unnoticed. However, if the bladder descends more severely, the symptoms can be more noticeable. Women affected by bladder prolapse often describe a foreign body sensation in the vagina or pain during sexual intercourse. Depending on the severity of the prolapse, the sensations range from an unpleasant feeling of pressure in the lower abdomen to pulling lower abdominal pain and radiating back pain. Affected women are also more susceptible to bladder infections.
Foreign body sensations, pressure and pain occur mainly when walking, standing, sitting, bending over and during bowel movements. When lying down, the symptoms often subside because the pressure of the overlying organs on the bladder is reduced and the bladder can retract slightly. As a result, the symptoms are typically less pronounced in the morning than in the evening.
Bladder function can also be affected by bladder prolapse, as the bladder and urethra can no longer fully perform their function without sufficient fixation to the pelvis.
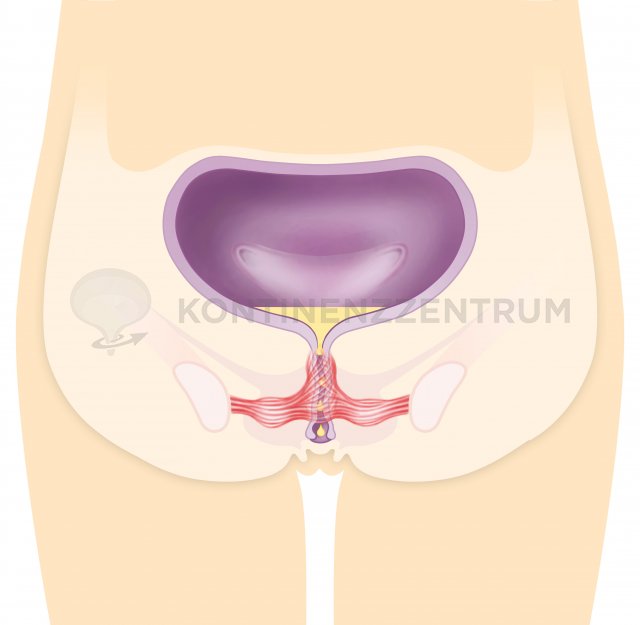
The pelvic floor stabilizes the bladder in the pelvis
The loosening of the urethral ligaments in particular can result in incontinence when coughing and during physical activity (so-called stress incontinence): Whenever the pressure in the abdomen is increased by a coughing jolt, lifting a shopping bag or during sport, this pressure wave propagates to the bladder and increases the pressure there too. Normally, an automatic closure of the urethra prevents the bladder from leaking. However, if the urethra lacks sufficient stability, this closure reflex fails, resulting in involuntary leakage of urine with or without an accompanying urge to urinate.
Diagnosis of bladder prolapse
If bladder prolapse is suspected, urology or urogynaecology is the specialist department responsible. Even if a gynecologist occasionally discovers the condition, a urologist should be consulted for a definitive diagnosis and treatment. The doctor will first conduct a thorough interview with the patient. The medical history will include questions about feelings of prolapse, protrusion in the vaginal area, urinary or bowel problems, number and course of births, micturition, physical activity and, if applicable, sexual intercourse.
Since the observation or description of a protrusion does not yet indicate which organs of the pelvis have descended or prolapsed, further examinations are carried out to diagnose bladder prolapse. These range from palpation of the abdominal cavity and the use of a two-part speculum to imaging procedures such as ultrasound of the urinary tract or cystoscopy.
During an ultrasound examination, the function of the bladder and urethra in women can be examined through the vagina. The length of the urethra and its angle to the bladder are measured, first at rest and then when pressing and coughing. This reveals whether bladder prolapse is the cause of incontinence. Urodynamic functional examinations can also be carried out to identify possible causes of incontinence or bladder dysfunction.
Therapy: Treatment options for bladder prolapse
 Bladder prolapse associated with symptoms often requires treatment, regardless of the age of the person affected. An improvement or even a spontaneous cure cannot be expected.
Bladder prolapse associated with symptoms often requires treatment, regardless of the age of the person affected. An improvement or even a spontaneous cure cannot be expected.
The treatment of bladder prolapse depends on the severity and, above all, the individual cause of the prolapse. Regardless of the severity of the condition, any form of bladder prolapse that bothers a woman and impairs her quality of life should be investigated and treated. This is the case, for example, if she feels a foreign body sensation in the vagina, if problems occur during sexual intercourse or if bladder emptying is impaired.
Conversely, not every bladder prolapse needs to be treated if the woman concerned has no symptoms.
There are two methods for treating bladder prolapse: conservative therapies and surgery.
- Conservative (non-surgical) treatment options include pelvic floor training, local hormone administration and the use of pessaries or special vaginal tampons.
Weight loss can also be part of the treatment plan if you are overweight. - Surgical treatment options include a variety of modern, low-complication operations, such as the Da Vinci operation, in which organs in the pelvis are lifted and stabilized.
An individually tailored surgical plan is developed for each patient based on the most precise and accurate preliminary examinations.
Pelvic floor exercises for bladder prolapse
Under the guidance of a physiotherapist, patients can specifically strengthen their weakened pelvic floor. Long-term pelvic floor training can stabilize mild bladder prolapse and prevent or improve stress incontinence. This can greatly improve the quality of life of those affected and delay a worsening of the condition. Pelvic floor therapy is a long-term project, short-term success cannot be achieved.
Pessary therapy for bladder prolapse
Pessary therapy can provide short-term improvement in symptoms and is usually used as a temporary treatment. A pessary - usually a soft ring or cube made of silicone - is placed in the vagina. The patient can remove, clean and reinsert the pessary herself at regular intervals. It does not hinder her when going to the toilet, but must be removed for sexual intercourse. Due to its position, the pessary can hold back the prolapsed bladder and other pelvic organs, but cannot permanently correct a prolapse. The advantage of this method is that no side effects or complications are to be expected if it is used and cared for correctly.
Bladder prolapse surgery
If the bladder prolapse is particularly pronounced or cannot be controlled by conservative measures, a number of surgical procedures can be considered. The lowered bladder can be lifted in different ways and fixed back into the pelvis. The choice of surgical method requires experience on the part of the doctor and is always individually tailored to the patient. The aim of the surgical procedure is to reconstruct the original position of the prolapsed bladder, thus alleviating the prolapse symptoms and restoring normal bladder or bowel function.
In many cases, the operation is carried out through the vaginal opening, for example in the case of prolapse of the bladder and bowel as a shortening of the anterior or posterior vaginal wall. If the uterus or vagina is lowered at the same time, the uterus may need to be secured in the pelvis by means of a suture on a fixed band deep in the pelvis or the uterus may need to be removed (only if family planning has been completed).
In the case of combined prolapse, an abdominal incision may also be useful. A mesh is attached to the anterior and posterior vaginal wall and fixed to the sacrum. If a relapse occurs after surgery for prolapse, a mesh insertion from the vagina can also be considered.
For more severe cases, minimally invasive DaVinci surgery is a reliable option. In this procedure, the surgeon operates using robot-assisted technology. Surgical instruments are attached to the arms of the robot, which carry out the operation directly by means of predefined movements from the control console. According to the manufacturer, over five million operations have been performed worldwide using the DaVinci system, meaning that this surgical procedure has long since become a reality.
Prevention of bladder prolapse
A healthy lifestyle, exercise and a normal body weight are the best tools for a strong pelvic floor and therefore a good prophylaxis against bladder and organ prolapse. In general, bladder prolapse cannot be prevented, but a timely visit to the doctor and early treatment can make a significant contribution to improving the condition and thus increasing quality of life.
Find out now about the diagnosis and treatment of bladder prolapse
Contact us if you would like a detailed consultation. We will be happy to inform you about your individual assessment and treatment options for bladder prolapse. You can reach our center (KontinenzZentrum Hirslanden) in Zurich at Tel. +41 44 387 29 10 from Monday to Friday between 8 a.m. and 5 p.m. You can also use our online appointment booking!
